- Phone : +770-996-0700
- Email : info@atlantaeyeconsultants.com
- Opening Hours : 08:00AM to 21:00PM
Macular Pucker
Home > Blog
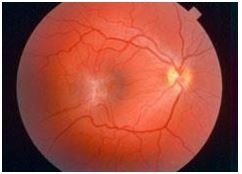
What is a macular pucker?
A macular pucker is scar tissue that has formed on the eye’s macula, located in the center of the eye’s light-sensitive tissue called the retina. The macula provides the sharp, central vision we need for reading, driving, and seeing fine detail. A macular pucker can cause blurred and distorted central vision.
Macular pucker is also known as epiretinal membrane, preretinal membrane, cellophane maculopathy, retina wrinkle, surface wrinkling retinopathy, premacular fibrosis, and internal limiting membrane disease.
Frequently Asked Questions about Macular Pucker
Is a macular pucker the same as age-related macular degeneration?
No. A macular pucker and age-related macular degeneration are two separate and distinct conditions, although the symptoms for each are similar. An eye care professional will know the difference.
Can macular pucker get worse?
For most people, vision remains stable and does not get progressively worse. Usually macular pucker affects one eye, although it may affect the other eye later.
Is a macular pucker similar to a macular hole?
A macular pucker and a macular hole are different conditions, although they both result from the same reason: The pulling on the retina from a shrinking vitreous. When the “pulling” causes microscopic damage, the retina can heal itself; scar tissue, or a macular pucker, can be the result. If the shrinking vitreous pulls too hard, it can tear the retina, creating a macular hole, which is more serious. Both conditions have similar symptoms – distorted and blurred vision. Also, a macular pucker will not “develop” into a macular hole. An eye care professional will know the difference.
Cause
What causes a macular pucker?
Most of the eye’s interior is filled with vitreous, a gel-like substance that fills about 80 percent of the eye and helps it maintain a round shape. The vitreous contains millions of fine fibers that are attached to the surface of the retina. As we age, the vitreous slowly shrinks and pulls away from the retinal surface. This is called a vitreous detachment, and is normal. In most cases, there are no adverse effects, except for a small increase in floaters, which are little “cobwebs” or specks that seem to float about in your field of vision.
However, sometimes when the vitreous pulls away from the retina, there is microscopic damage to the retina’s surface (Note: This is not a macular hole). When this happens, the retina begins a healing process to the damaged area and forms scar tissue, or an epiretinal membrane, on the surface of the retina. This scar tissue is firmly attached to the retina surface. When the scar tissue contracts, it causes the retina to wrinkle, or pucker, usually without any effect on central vision. However, if the scar tissue has formed over the macula, our sharp, central vision becomes blurred and distorted.
Symptoms
What are the symptoms of a macular pucker?
Vision loss from a macular pucker can vary from no loss to severe loss, although severe vision loss is uncommon. People with a macular pucker may notice that their vision is blurry or mildly distorted, and straight lines can appear wavy. They may have difficulty in seeing fine detail and reading small print. There may be a gray area in the center of your vision, or perhaps even a blind spot.
Treatment
How is a macular pucker treated?
A macular pucker usually requires no treatment. In many cases, the symptoms of vision distortion and blurriness are mild, and no treatment is necessary. People usually adjust to the mild visual distortion, since it does not affect activities of daily life, such as reading and driving. Neither eye drops, medications, nor nutritional supplements will improve vision distorted from macular pucker. Sometimes the scar tissue–which causes a macular pucker–separates from the retina, and the macular pucker clears up.
Rarely, vision deteriorates to the point where it affects daily routine activities. However, when this happens, surgery may be recommended. This procedure is called a vitrectomy, in which the vitreous gel is removed to prevent it from pulling on the retina and replaced with a salt solution (Because the vitreous is mostly water, you will notice no change between the salt solution and the normal vitreous). Also, the scar tissue which causes the wrinkling is removed. A vitrectomy is usually performed under local anesthesia.
After the operation, you will need to wear an eye patch for a few days or weeks to protect the eye. You will also need to use medicated eye drops to protect against infection.
How successful is this surgery?
Surgery to repair a macular pucker is very delicate, and while vision improves in most cases, it does not usually return to normal. On average, about half of the vision lost from a macular pucker is restored; some people have significantly more vision restored, some less. In most cases, vision distortion is significantly reduced. Recovery of vision can take up to three months. Patients should talk with their eye care professional about whether treatment is appropriate.
What are the risks of surgery?
The most common complication of a vitrectomy is an increase in the rate of cataract development. Cataract surgery may be needed within a few years after the vitrectomy. Other, less common complications are retinal detachment either during or after surgery, and infection after surgery. Also, the macular pucker may grow back, but this is rare.
Current Research
What research is being done?
Research studies are being conducted to determine other treatments for macular pucker. Please note that both of the procedures described below need additional clinical testing. We suggest you share this information with your eye care professional.
Some physicians are researching the use of a surgical procedure in which scar tissue is peeled off without performing the vitrectomy.
Other doctors are researching a new surgical technique to remove the internal limiting membrane (a layer of the retina) for patients with both macular pucker and macular hole. This surgical technique is called Fluidic Internal Limiting Membrane Separation (FILMS). After a vitrectomy, fluid is injected between the membrane and the retina that causes the membrane, along with the scar tissue, to lift away. It is then removed with forceps.
Source: National Eye Institute of National Institutes of Health
Latest Blog & News letter
download & read
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus.
